https://www.washingtonpost.com/business/2021/12/09/long-covid-work-unemployed/
Long covid is destroying careers, leaving economic distress in its wake
- Spoiler:
By Christopher Rowland
Yesterday at 10:23 a.m. EST
Before the coronavirus ruined her plans, Tiffany Patino expected to be back at work by now. She and her boyfriend intended to move out of a basement in suburban Maryland, where his grandmother lets them stay for free, so they could raise their infant son in a place of their own. Maybe get a new car.
But Patino got sick with covid-19 more than a year ago. Instead of getting better, chronic exhaustion and other symptoms persisted, delaying her return to a restaurant job and swamping her goal of financial independence. After reaching what she calls her “hell-iversary” last month, Patino remains unable to rejoin the workforce. With no income of her own, she’s exhausted, racked with pain, short of breath, forgetful, bloated, swollen, depressed.
At 28 years old, she can barely take her baby to the playground. “I go on a walk, and I have to use the stroller like a walker,” she said. “Whatever life I have right now, it’s more like surviving. I’m not living my dream. I’m living a nightmare.”
Across America, many of the nearly 50 million people infected with the coronavirus continue to suffer from some persistent symptoms, with a smaller subset experiencing such unbearable fatigue and other maladies that they can’t work, forcing them to drop out of the workforce, abandon careers and rack up huge debts.
Hard data is not available and estimates vary widely, but based on published studies and their own experience treating patients, several medical specialists said 750,000 to 1.3 million patients likely remain so sick for extended periods that they can’t return to the workforce full time.
The days of full covid coverage are over. Insurers are restoring deductibles and co-pays, leaving patients with big bills.
Long covid is testing not just the medical system, but also government safety nets that are not well suited to identifying and supporting people with a newly emerging chronic disease that has no established diagnostic or treatment plan. Insurers are denying coverage for some tests, the public disability system is hesitant to approve many claims, and even people with long-term disability insurance say they are struggling to get benefits.
Employers are also being tested, as they must balance their desire to get workers back on the job full time with the realities of a slow recovery for many patients.
“They are suffering in dramatic ways, and in ways that have altered their lives and placed them in financial peril,” said Harlan Krumholz, a cardiologist and scientist at Yale University and Yale New Haven Hospital.
For these three long haulers, debilitating symptoms and fatigue has kept them from returning to work — and in return, struggling to navigate their new normal. (Drea Cornejo, Joy Yi, Colin Archdeacon/The Washington Post)
The Washington Post interviewed more than 30 people around the country experiencing the sudden financial slide caused by the long form of the disease. They have been laid off and fired, quit jobs, shuttered businesses. They described falling behind on rent, mortgages and car payments. Some worried about losing their housing.
Depression and anxiety that are part of the brutal mix of long covid symptoms are exacerbated by despair over vanishing income. From health-care professionals and small-business operators to government employees and warehouse supervisors, the patients expressed fears about never being able to return to work.
Often referred to as “long haulers,” they experience mild symptoms to begin with, then get stuck with months of chronic fatigue, shortness of breath, confusion and memory loss, erratic and racing heartbeats, radical spikes in blood pressure, painful rashes, shooting pains and gastrointestinal problems.
The government calls it post-acute sequelae of SARS-CoV-2, or PASC. The National Institutes of Health is spending $1.15 billion to study the syndrome. The symptoms sometimes subside, lulling long haulers into a false sense of relief, only to come roaring back after performing simple chores like vacuuming a living room or raking leaves.
Patino is afraid to carry her son for too long, worried she will drop him. She takes naps every day. If she did return to work as a server or host in a restaurant, she fears she would quickly get fired for missing work.
“I just feel so old. I feel so tired. When you are dealing with so many symptoms, every day it’s like a lottery pick,” Patino said.
Doctors treating long haulers say the symptoms cut across race and class lines.
‘I just pray God will help me’: Racial, ethnic minorities reel from higher covid-19 death rates
“I have hundreds of patients who have had to take time off for long periods of time, quit their jobs, or get fired from their jobs, or take lesser-paying jobs” because of long covid, said Janna Friedly, vice chair for clinical affairs at the Department of Rehabilitation Medicine at the University of Washington School of Medicine, where she and her team are helping long haulers build strength and return to work.
On top of the loss of income, some patients lose their employer-sponsored health insurance when they can’t work. “I’ve seen patients who have gone from fully insured to not being able to come back and see me in clinic in the middle of our treatment because they have lost their job and no longer can afford to seek care,” Friedly said.
Even for those who do have insurance, treating long covid can be unusually complicated and costly, since it’s a new disease without an established diagnostic or treatment plan and coverage for certain tests may be denied.
Health insurance companies, citing the blizzard of tests being ordered, say they are waiting for data-driven protocols to emerge so they can match insurance coverage with the best testing and treatment strategies for long covid.
“In many cases, the kitchen sink approach is not helping,” said Michael Sherman, chief medical officer of Point32Health, a nonprofit insurance company in Massachusetts formed from the merger of Harvard Pilgrim and Tufts health plans. Until research is published into what tests and treatments work, he said, “there’s a lack of evidence that anyone can look to.”
‘This virus took my career’
The cognitive and emotional impacts also make it difficult for patients to navigate the bureaucratic tangles required to keep health insurance and file disability claims after a job loss.
John Buccellato, 64, an emergency medicine doctor at an urgent care clinic on Manhattan’s Upper East Side, was hospitalized with the virus in March 2020, in the same hospital where his mother died of covid.
In a matter of days, he went from treating patients at a busy clinic to being engulfed in a health crisis as covid attacked his lungs and vascular system. Severe cognitive and emotional strain left him unable to manage his day-to-day affairs.
Overwhelmed by brain fog and the sense of loss over his career, he frequently sobbed on the phone as he described his struggles in an interview, including the loss of his employer-sponsored insurance.
A clinical neuropsychologist treating him, Gudrun Lange, said Buccellato experienced brain bleeds and a tumor. He repeats himself and seems easily confused.
“He starts getting emotional, involuntary crying, and there’s nothing he can do about it,” she said.
Buccellato said he has tens of thousands of dollars in unpaid medical bills that accumulated when he first lost his health insurance. He has some property and savings, but no weekly cash flow, he said. He signed up for COBRA, which provides a continuation of health insurance after a job loss, but after congressionally approved waivers that made it free expired in September, it now costs $922 a month, he said.
Garage operators briefly impounded his Lexus because he could no longer pay the $400 a month to park the car, he said. Now it’s on the street, accumulating tickets.
Treatments will change the pandemic, but they can’t end it alone
Buccellato said he recognizes his career is prematurely over, but he can’t figure out how to dig himself out of his worsening financial predicament. A lawyer helped him file a disability claim with the Social Security Administration, which a member of his support team said was recently successful. Because he left work for medical reasons, he was not eligible for unemployment insurance.
“This virus took my career away. I can’t do anything in the medical field right now. Nobody is going to hire me,” he said.
Other patients who experienced a similar plunge in income with the loss of their professional careers described their new reliance on government aid.
Chimere Smith, 39, a middle school teacher in Baltimore who has testified in Congress about covid’s impact on her life, has not worked since she caught the virus in the early weeks of the pandemic.
She has blown through $12,000 in savings and is on food stamps.
She said the sense of loss is profound because she worked her way up from a childhood in a poor area of Washington, D.C. Before she got sick, she had hoped to become a school principal.
“I was following the trajectory of what I was told for years to be successful and Black in the world,” she said, “and to have it all taken away by illness is a loss that I don’t think I’ll ever recover from. Even using the word devastation doesn’t really capture the full scope of my experience.”
She also plans to apply for disability assistance.
But many patients applying for disability insurance benefits are initially denied and require lengthy appeals, according to patients, doctors and lawyers, in part because the medical community is still grappling with how to diagnose their symptoms.
The Social Security Administration said in an email that it has received 16,000 covid-related disability claims since December 2020, but the agency would not disclose how many of those were approved or denied.
Patients, advocates and lawyers said private disability insurers, which offer long-term disability coverage through employee benefit plans, have also been denying many claims.
For individuals who said they can’t work, the denials are frustrating. Michael Heidenberg, 48, of White Plains, N.Y., was unable to return to his $60,000 a year job as an academic adviser at Berkeley College, a regional for-profit college that kept him on for four weeks beyond the 12 weeks of unpaid leave required by the Family Medical Leave Act requirement. The college said it could not keep him on the books longer because it would create a hardship for his department, he said.
Heidenberg had purchased long-term disability insurance through his former employer, which promised a benefit of $3,100 a month, up to $150,000.
But Reliance Standard, the insurance carrier, recently denied his first application, saying he could do his job sitting down.
Heidenberg said that does not take into account his inability to concentrate for long periods and the dangerous spikes in his blood pressure since he contracted covid last year. Asked to discuss the denial, Reliance Standard said it would not comment on an individual claimant.
While he prepares for an appeal, Heidenberg said he and his wife, Alexis, are trying to figure out how to keep their apartment, which costs $1,700 a month, and cover COBRA health insurance, which is $1,200. He opted for COBRA over Medicaid or the Affordable Care Act exchanges because COBRA covers all the doctors he needs, he said.
“Finding doctors who are well-versed in treating post-covid patients has been incredibly difficult,” Heidenberg said.
Still, his COBRA eligibility will expire in March 2022 and he will need to find new insurance. Mike and Alexis have a GoFundMe page, which has raised $12,000. Alexis receives $988 a month in federal disability benefits because of a fibromyalgia diagnosis. That is currently their only income.
If they have to sell their apartment, they fear they will be priced out of White Plains, where they both grew up. Heidenberg expects his financial problems will get worse.
“It’s just this incredibly scary freight train coming right at us,” Heidenberg said. “You blame yourself. I was the primary breadwinner, and now we’re struggling because I got sick.”
In Kaufman, Tex., a small town 20 miles outside of Dallas, Angie Smith, 44, has slipped behind on $750-a-month payments on her Nissan Frontier pickup truck, which she bought when she was making more than $50,000 a year as an orthodontist assistant.
She said she was laid off in March 2020. She got covid eight months later and has been plagued by fatigue, shortness of breath, joint pain and spikes in body temperature ever since.
Unemployment checks that kept her financially afloat ended in September.
She said she had $150 in her checking account in mid-November and $1,400 in rent due in December. Friends from church have helped her hunt for jobs she can do over the phone from home.
“If I lose my house, then I could possibly set up my computer at someone’s house. If I lose my truck, I can still work from home,” she said. “I have so many of these scenarios going on in my head that I don’t know what to do.”
Nearly all of the patients interviewed by The Post said they wanted to return to work but could not figure out how to get back on the path to productivity.
“Employers are not used to dealing with this kind of work situation. Patients are often told, ‘Just come back when you’re 100 percent,’ which could be a really long time out,” said Greg Vanichkachorn, a family physician and occupational medicine specialist at the Mayo Clinic who is treating long-haul patients.
Employers and patients need to understand that many long haulers should return to work on a limited, part-time basis, perhaps working from home, while they slowly work on building strength, he said.
Seattle resident Eileen Hood thought she was ready to begin earning money again.
Hood got sick with covid in October 2020, forcing her this year to close the small business she had run with a friend for 15 years, selling wigs, specialized clothing and other needs for cancer patients. Hood’s attempt to return to the job she loved ended in frustration.
“Forty minutes into my last wig-fitting, with a lovely lady, I just simply did not have enough air or energy to finish,” she said.
The $70,000 per year she drew from the shop has evaporated, cutting her family’s income in half.
She is 53 years old and wants to get back to work. Hood said she went to a job interview in October but was forced to cancel her appointment for the second interview in November.
“I went out and raked some leaves and made dinner for my family, and the next day, I couldn’t get out of bed,” she said. “It’s the roller coaster of living with long covid.”
Feeling ‘worthless’
At the onset of the shutdowns in March 2020, Patino lost her job as a server at Firebirds Wood Fired Grill in suburban Maryland. Her boyfriend was laid off from another restaurant around the same time.
“We had to sign up for unemployment, and I was pregnant,” Patino said.
Two months after the September birth of her baby, Leon, she tested positive for the coronavirus.
Her symptoms were moderate, but she could no longer nurse her baby. She was first told she was probably suffering from postpartum depression, she said. She went for a second opinion and staff found signs of the classic “ground-glass” pneumonia in her lungs, she said.
“Almost a month later, right before Christmas, I was still feeling crappy, still feeling tired,” she said. By January, she went back to the hospital and was told she might be a “long hauler.”
“The doctor’s like, ‘In a few months, by March, by April, by the summer, you should be much better,’ ” Patino said.
But as summer passed into fall, with no more unemployment checks and winter approaching, her symptoms persisted, some of them strange: “I got my taste back and smell is still iffy. It comes and goes. I will smell smoke; I will smell gasoline. Sometimes I smell feces.”
Patino said she endures an isolated and depressing existence, knowing that many people are returning to normal while her plans remain on hold. She has considered trying an office job where she could work while seated but worries she would have to call in sick too often. Getting an apartment and a new car to replace their 2007 Kia remain out of reach, she said.
“I just feel like kind of a worthless person,” she said. “I can’t even do something like taking care of my child, cooking dinner, doing laundry and typical stay-at-home mom stuff.”
With long covid, she said, “my world shattered, and everything just came crumbling down.”
Virus
- Posts : 7233
Join date : 2019-11-04
- Post n°201
 Re: Virus
Re: Virus

- Posts : 52540
Join date : 2017-11-16
- Post n°202
 Re: Virus
Re: Virus

- Posts : 11340
Join date : 2014-10-28
- Post n°203
 Re: Virus
Re: Virus
_____
most of us probably not getting better
but not getting better together

- Posts : 13817
Join date : 2016-02-01
- Post n°205
 Re: Virus
Re: Virus
Hospitalizacije 2512 vs 1990 (rast od 26% - odgovara vremenu dupliranja od oko 6 dana)
Na kiseoniku 331 vs 280 (rast od 18% - odgovara vremenu dupliranja od oko 8 dana)
Na respiratoru 69 vs 58 (rast od 19% - odgovara vremenu dupliranja od oko 8 dana)
Broj umrlih za dva dana: 54, tj. dnevni prosek 27
Broj umrlih za 10 dana pre toga: 124, tj. dnevni prosek 12,4
I smrtnost očigledno raste.
Izvor:
https://www.nicd.ac.za/diseases-a-z-index/disease-index-covid-19/surveillance-reports/daily-hospital-surveillance-datcov-report/
Slike u spoileru:
- Spoiler:



Raspodela ovih 54 umrlih u zadnja dva dana po starosnim grupama:
0-9: 2
10-19: 1
20-29: 1
30-39: 6
40-49: 8
50-59: 7
60-69: 7
70-79: 8
80+: 14

- Posts : 13817
Join date : 2016-02-01
- Post n°206
 Re: Virus
Re: Virus
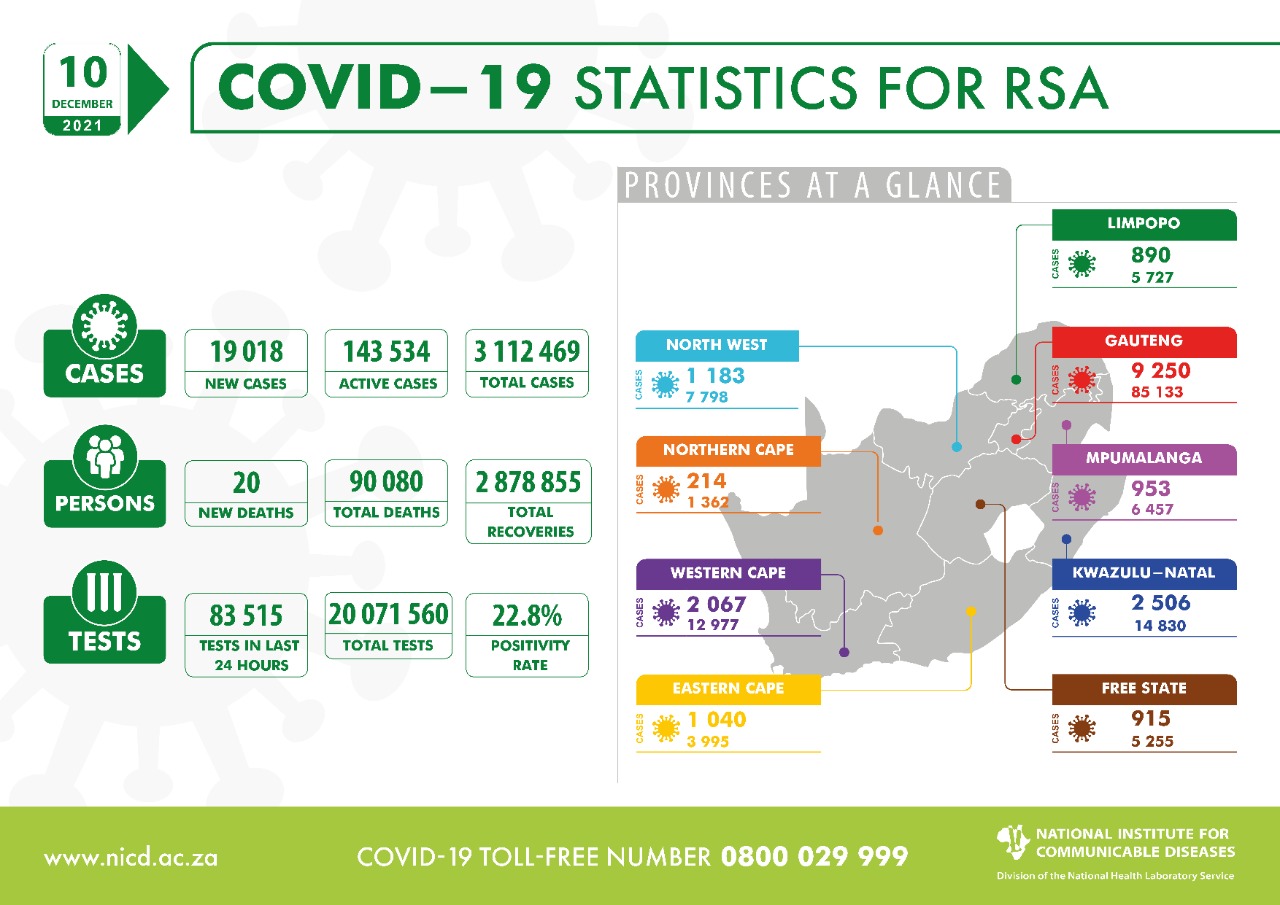
https://twitter.com/nicd_sa/status/1469400938964307969
https://twitter.com/nicd_sa/status/1466814557154906116

- Posts : 13817
Join date : 2016-02-01
- Post n°207
 Re: Virus
Re: Virus
- Spoiler:
Mia Malan, 21h, 18 tweets, 12 min read
Update on #Omicron in SA via @Dr_Groome from @nicd_sa (presented @ Fri's @heatlhza press briefing):
[Thread]
1. The 7 day moving average of new #COVID19 cases = increased 40-fold between 16 Nov (332) + 8 Dec (13,237)
2. This increase is much steeper than in any previous wave
2. @Dr_Groome:
1. The increase in new #COVID19 cases = mostly driven by Gauteng, where the #Omicron outbreak started
2. Left graph = absolute nr of cases, right graph = incidence (new cases), accounted for population size = starting to see increases in other provinces too
3. What do new #COVID19 cases look like by age?
1. Early on in the #Omicron wave we saw more cases in younger age groups
2. Currently, the incidence is highest in the 20-39 year and 40-59 year group, followed by the 60+ year group
4. @Dr_Groome:
There has been a dramatic increase in the test positivity rate (the % of tests that come out positive) - this increase is steeper than in any previous wave:
- Between 14 + 28 Nov the + rate increased from 2.5% to 24.9%
- Yesterday (Thu), the + rate was: 29.8%
5. @Dr_Groome:
1. This is how positivity test rates are distributed across SA (red = over 30%)
2. See how the red is concentrated in the north of SA in Gauteng, but is now filtering to the rest of the country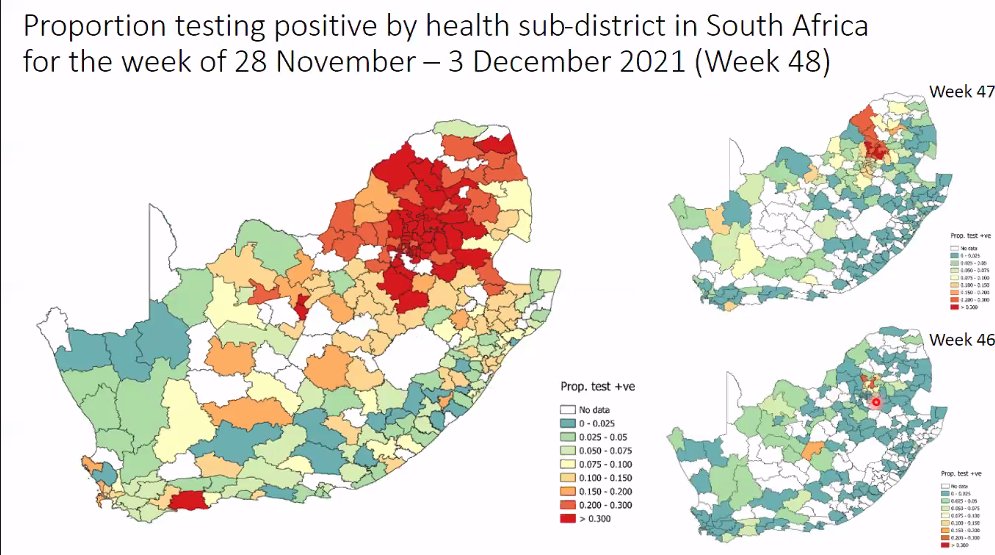
6. @Dr_Groome:
1. This is a table of test positivity rates for provinces
2. Gauteng's (35%) + rate is the highest (where the #Omicron outbreak in SA started), followed by Northwest, MP and Limpopo (all 3 = neighboring provinces of GP)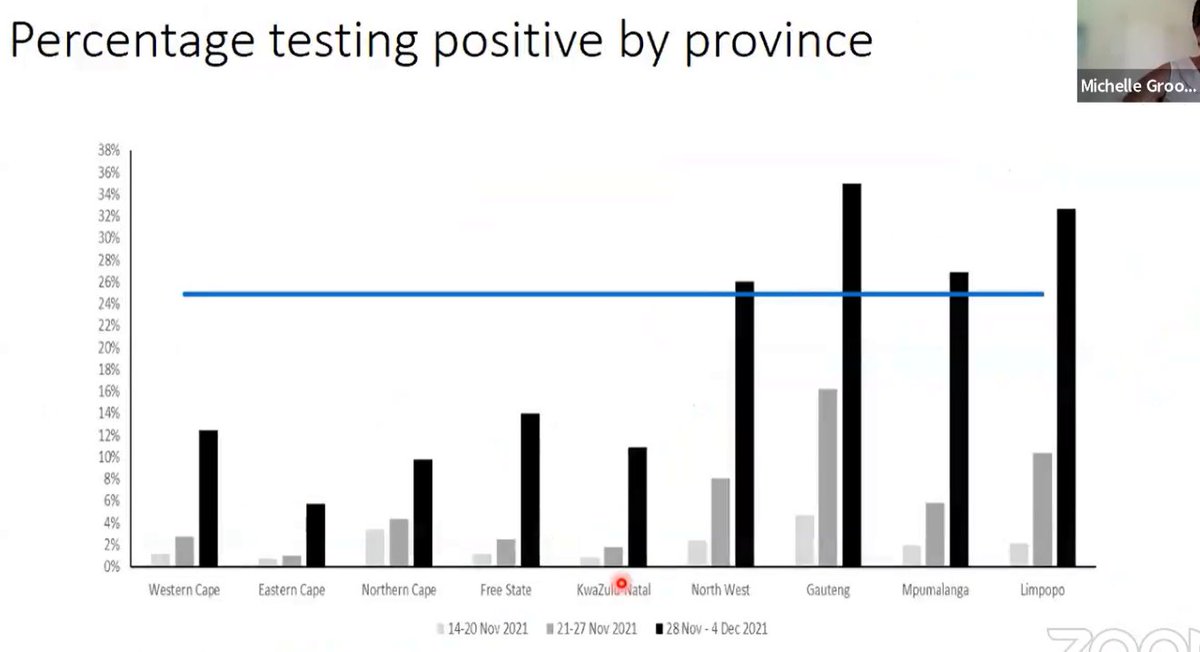
7. Which SA provinces have officially entered a 4th wave?
@Dr_Groome:
1. Gauteng
2. Northwest
3. Mpumalanga
8. What's happening with reproductive (R) numbers? (This is how many other people 1 infected person will infect):
1. Nationally our R nr = 2.55 (this is the highest R nr SA has seen since the start of #COVID19)
2. In Gauteng (where SA's #Omicron outbreak started) the R nr = 3.06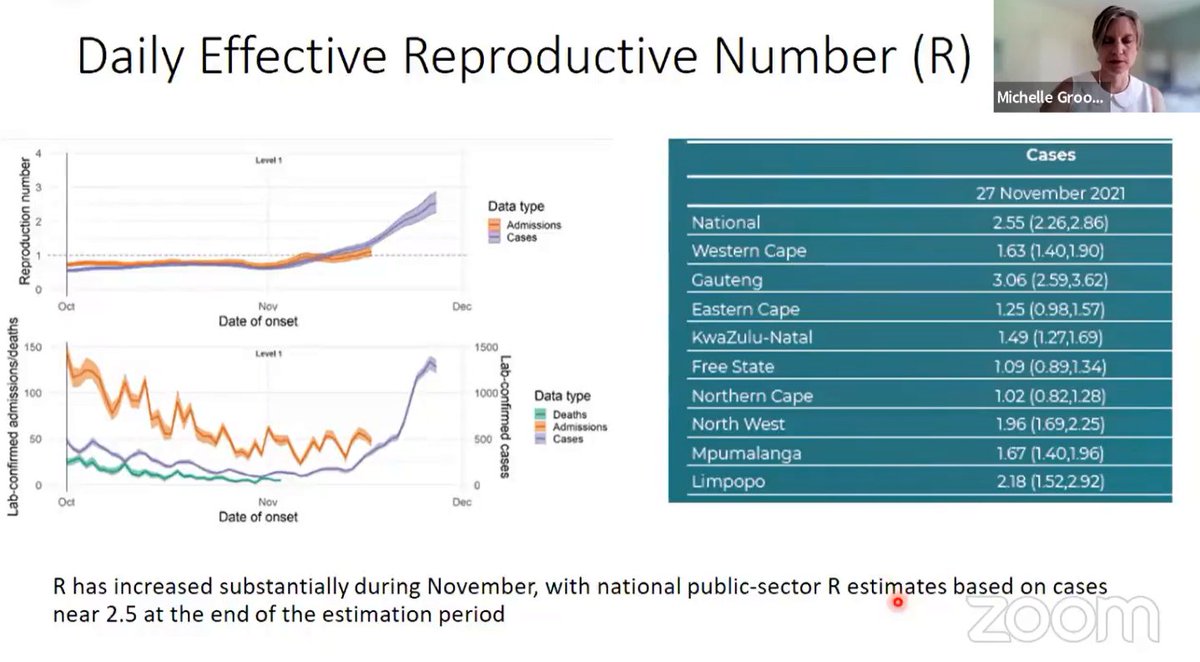
9. What's happening with hospitalisations?
1. The right graph shows the increase in hospitalisations in both the private and public sector
2. The left graph shows a drop off, but that is due to a delay in the reporting of cases, not an actual drop in cases
10. The left graph compares the nr of new cases (orange) with hospital admissions (grey) for all waves:
The diffs with the 4th (#Omicron) wave = admissions start later (a while after a steep increase in cases; admissions in previous waves = along with an increase in cases).
11. Early indications of #Omicron hospitalisations, based on SA data:
1. We're starting to see a disconnect between cases and hospitalisations
2. Right graph = there is a much lower % of patients getting admitted (blue) - but could be because it's still early in the wave
12. What's happening with #COVID19 deaths?
1. We haven't seen any significant increase nationally
2. We're starting to see small increases in Gauteng (where SA's #Omicron outbreak started)
13. This table shows increases in #COVID19 hospital admissions/deaths in provinces:
1. Gauteng: Increase from an average of 32.57 (for 2 weeks) to 181.07 (the average of the following 2 weeks) = 455% increase
2. Deaths in Gauteng = 68% increase
14. AGE breakdown 4 GAUTENG admissions (last 3 weeks):
1. We started off with a larger % of admissions in younger (20/below) groups, but that is now changing
2. We're now seeing the % of younger admissions decreasing + the % of admissions in older groups (slightly) increasing
15. GAUTENG admission data broken down into smaller age bands:
1. 0-5 years = a high % of admissions initially, but this has decreased from 14% of admissions to 7% of admissions over the last 3 weeks
2. 60+ admissions have increased from about 13% to just over 16%
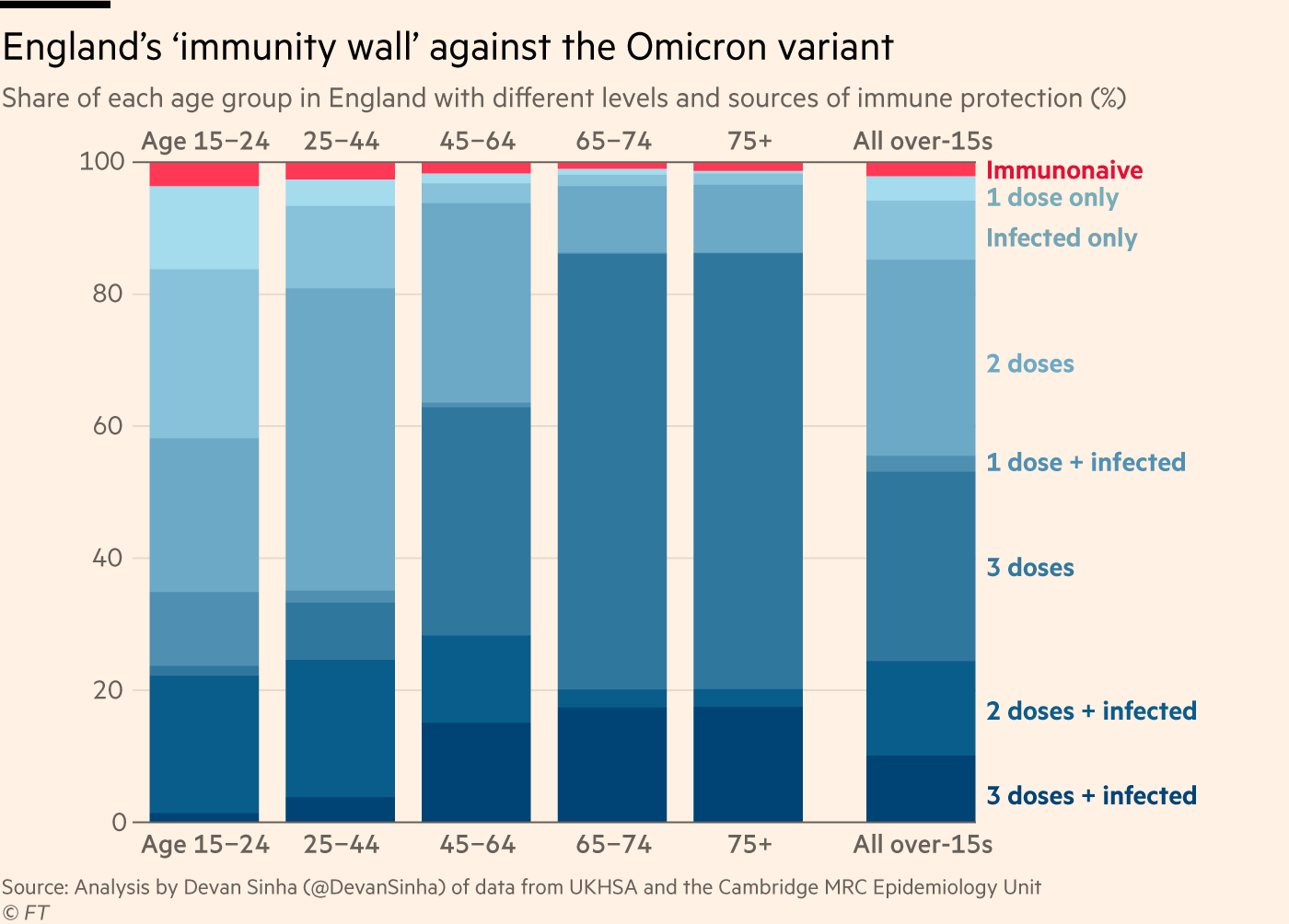
16. @Dr_Groome:
1. This graph shows that the #COVID19 admissions we're seeing are mostly among the age groups with low vaccination rates
2. This is in line with evidence that vaccines protect people from falling severely ill with COVID (so they don't need hospitalisation)
17. What is defined as severe illness?
= People with acute respiratory distress syndrome, those needing oxygen or are admitted to ICU
Note: The data presented = early stage data, which means many beds = still available + docs are more likely to admit patients with mild disease
18. Summary:
1. The nr of new #COVID19 cases are on a sharp increase and so is the test positivity rate
2. % of younger admissions = changing (becoming a smaller % of total admissions)
3. No signals of more severe disease
4. Most hospital admissions = unvaccinated people
- Posts : 10414
Join date : 2020-06-19
- Post n°208
 Re: Virus
Re: Virus
_____
Međuopštinski pustolov.
Zli stolar.

- Posts : 52540
Join date : 2017-11-16
- Post n°209
 Re: Virus
Re: Virus
- toliko sam verovao u tebe, sto me nisi spasio
- kako nisam, organizovao sam onolike ljude da naprave vakcinu

- Posts : 13817
Join date : 2016-02-01
- Post n°210
 Re: Virus
Re: Virus

https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1040064/9_December-2021-risk-assessment-for-SARS_Omicron_VOC-21NOV-01_B.1.1.529.pdf

- Posts : 13817
Join date : 2016-02-01
- Post n°211
 Re: Virus
Re: Virus
COVID restrictions across the UK will be kept "under review" after the government was presented "with some very challenging new information" about Omicron, Michael Gove has said.https://t.co/lmYNcnTfzi pic.twitter.com/e2AO0H23zN
— Sky News (@SkyNews) December 11, 2021

- Posts : 13817
Join date : 2016-02-01
- Post n°212
 Re: Virus
Re: Virus
Update on coronavirus outbreak at Christmas party in Oslo:
— BNO Newsroom (@BNODesk) December 10, 2021
- 80 out of 111 participants later tested positive. All or most believed to be Omicron
- Everyone had a negative test before the event and nearly all were vaccinated
- 79 had symptoms, but no one was hospitalized

- Posts : 52540
Join date : 2017-11-16
- Post n°213
 Re: Virus
Re: Virus

- Posts : 13817
Join date : 2016-02-01
- Post n°214
 Re: Virus
Re: Virus
https://twitter.com/jburnmurdoch/status/1469427353117986829

- Posts : 13817
Join date : 2016-02-01
- Post n°215
 Re: Virus
Re: Virus
So, the UKHSA project ONE MILLION infections PER DAY based on reasonable assumption of a doubling time of Omicron of 2.5 days
— Dr Duncan Robertson (@Dr_D_Robertson) December 10, 2021
Not One Million by the end of the year:
ONE MILLION INFECTIONS
PER DAY
BY CHRISTMAS
The Government has not responded to thishttps://t.co/bpApPHFvMl pic.twitter.com/AgBtrp6wdT
https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1040076/Technical_Briefing_31.pdf (strana 28)

- Posts : 13817
Join date : 2016-02-01
- Post n°216
 Re: Virus
Re: Virus
rumbeando wrote:Nova zvanična britanska procena omikrona: ima prednost u širenju nad deltom sigurno zbog rezaražavanja tj. izbegavanja imuniteta stečenog vakcinisanjem ili preležavanjem delte i ranijih sojeva, ali možda i sam po sebi (tj. međunezaraženimapotpuno nezaštićenima)

- Posts : 13817
Join date : 2016-02-01
- Post n°217
 Re: Virus
Re: Virus
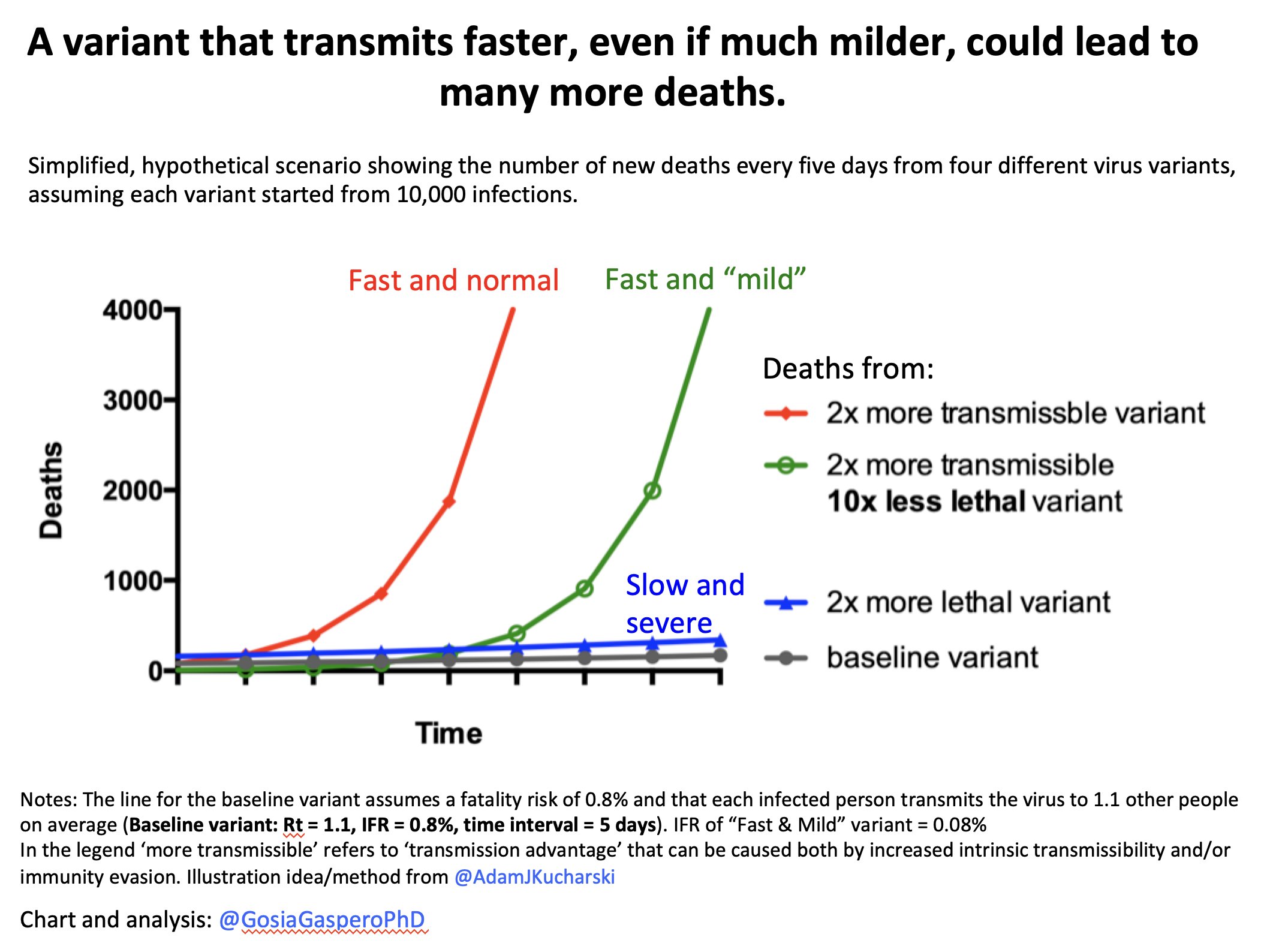
https://twitter.com/GosiaGasperoPhD/status/1469456805491138560

- Posts : 13817
Join date : 2016-02-01
- Post n°218
 Re: Virus
Re: Virus

South Africa is similarly timely in their sequence sharing. We can start by looking at the rate of increase of frequency of Omicron in South Africa and the UK. Here we see that frequency of Omicron has increased from ~0.1% on Nov 23 to almost 1% on Nov 29. 4/21 pic.twitter.com/wF5WdLVtkn
— Trevor Bedford (@trvrb) December 10, 2021
The vertical scale is a logit function.
— Dr Kevin Purcell
logit(p) = log(p/1 - p)
i.e the log of the odds.
It is the inverse of the logistic function so if you plot logistic growth on a logit scale you get a straight line.https://t.co/gPgpLe2xcE
(@kevinpurcell) December 10, 2021
Ha logit axes... I just did another one with S dropout data I was pasting together from various sources... Not looking good... pic.twitter.com/I6LC4FCU2l
— Tom Wenseleers (@TWenseleers) December 10, 2021

- Posts : 13817
Join date : 2016-02-01
- Post n°219
 Re: Virus
Re: Virus

https://www.cdc.gov/mmwr/volumes/70/wr/mm7050e1.htm?s_cid=mm7050e1_w

- Posts : 13817
Join date : 2016-02-01
- Post n°220
 Re: Virus
Re: Virus
https://news.sky.com/story/covid-19-omicron-could-cause-between-25-000-and-75-000-deaths-in-england-without-tougher-restrictions-experts-12492584COVID-19: Omicron could cause between 25,000 and 75,000 deaths in England without tougher restrictions - experts
The Omicron variant could cause between 25,000 to 75,000 deaths in England over the next five months if no additional measures are taken beyond Plan B, according to experts.
New modelling from the London School of Hygiene & Tropical Medicine (LSHTM) used experimental data to look at how Omicron may transmit as the country heads into 2022.
It suggests that Omicron could potentially cause more cases and hospitalisations in England than during the wave in January 2021, if additional control measures are not taken.
Under the best-case scenario, the variant could lead to a peak of more than 2,000 daily hospital admissions, with 175,000 hospitalisations and 24,700 deaths between 1 December 2021 and 30 April 2022, the projection suggests.
The optimistic scenario is one where Omicron's immunity escape is low and boosters prove highly effective.
Measures such as restrictions on indoor hospitality, closure of some entertainment venues, and limits on gathering sizes from early next year would be sufficient to substantially control this wave, reducing hospitalisations by 53,000 and deaths by 7,600, the experts say.
Under the worst-case scenario (high immune escape and lower effectiveness of boosters), if no additional control measures are taken, there could be 492,000 hospitalisations and 74,800 deaths.
In this scenario, the experts estimate that stronger measures may be required to keep the number of hospital admissions below the January 2021 peak.
Dr Rosanna Barnard, who co-led the research, said that while there is still a lot of uncertainty over Omicron, "these early projections help guide our understanding about potential futures in a rapidly evolving situation".
"In our most optimistic scenario, the impact of Omicron in the early part of 2022 would be reduced with mild control measures such as working from home," she said.
"However, our most pessimistic scenario suggests that we may have to endure more stringent restrictions to ensure the NHS is not overwhelmed.
"Mask-wearing, social distancing and booster jabs are vital, but may not be enough.
"Nobody wants to endure another lockdown, but last-resort measures may be required to protect health services if Omicron has a significant level of immune escape or otherwise increased transmissibility compared to Delta.
"It is crucial for decision-makers to consider the wider societal impact of these measures, not just the epidemiology."

- Posts : 13817
Join date : 2016-02-01
- Post n°221
 Re: Virus
Re: Virus

https://files.ssi.dk/covid19/omikron/statusrapport/rapport-omikronvarianten-10122021-ek56-version2

- Posts : 13817
Join date : 2016-02-01
- Post n°222
 Re: Virus
Re: Virus
https://www.jpost.com/health-and-wellness/coronavirus/israels-first-omicron-covid-case-i-am-still-weak-688107Ten days after Dr. Elad Maor was diagnosed as the country’s first Omicron variant COVID-19 patient, the cardiologist returned to work at Sheba Medical Center.
“I am still weak,” he told The Jerusalem Post on Tuesday from one of the hospital’s bustling cafeterias on his first day back.
Maor tested positive for COVID-19 on November 28 and was diagnosed as having the variant a few days later. He was fully vaccinated with three shots of the Pfizer coronavirus vaccine. (...)
The variant hit Maor harder than he expected, causing a fever for 48 hours and extreme fatigue for 72 hours. He said he had muscle aches, too. And even now, Maor said he is not feeling back to himself.

- Posts : 52540
Join date : 2017-11-16
- Post n°223
 Re: Virus
Re: Virus
rumbeando wrote:
https://twitter.com/GosiaGasperoPhD/status/1469456805491138560
Naravno

- Posts : 8696
Join date : 2016-10-04
- Post n°224
 Re: Virus
Re: Virus
Са ранијим сојевима је било више преминулих него хоспитализованих са омикроном.rumbeando wrote:1,4% hospitalizovanih među dosad zaraženima omikronom u Danskoj.
Што значи да ће донети неке мере отприлике кад буду десетине хиљада заражених дневно.

- Posts : 13817
Join date : 2016-02-01
- Post n°225
 Re: Virus
Re: Virus
rumbeando wrote:18 (1,4%) hospitalizovanih među dosad zaraženima omikronom u Danskoj.
Danci testiraju sve u 16, evo kako izgleda dnevni prosek broja testova na 1000 stanovnika usrednjen na nedeljnom nivou u Danskoj, Britaniji, Nemačkoj i Srbiji:

https://ourworldindata.org/explorers/coronavirus-data-explorer?zoomToSelection=true&facet=none&pickerSort=asc&pickerMetric=location&Metric=Tests&Interval=7-day+rolling+average&Relative+to+Population=true&Align+outbreaks=false&country=DNK~GBR~DEU~SRB
Last edited by rumbeando on Sat Dec 11, 2021 4:00 pm; edited 1 time in total


 by Del Cap Fri Dec 10, 2021 10:08 pm
by Del Cap Fri Dec 10, 2021 10:08 pm